Do you find yourself questioning why your body responds with flushing, itching, or swelling seemingly without reason? Ever experienced unexplained fatigue, headaches, or digestive issues that persist despite your best efforts?
These mysteries might find their roots in the intricate workings of mast cells.
What are Mast Cells?
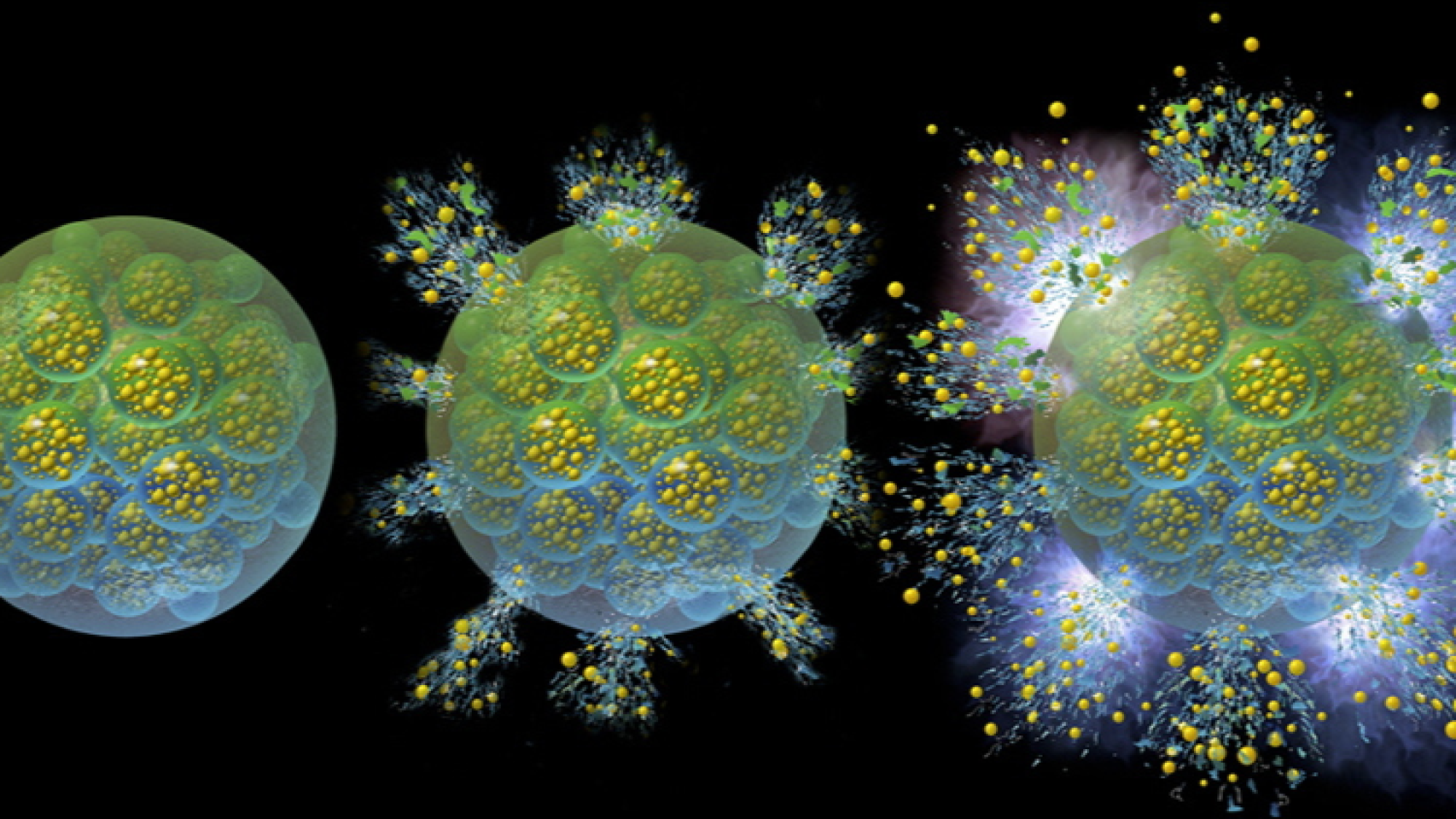
Mast cells are a vital part of our immune system, stationed throughout the body, especially in tissues prone to contact with the external environment. Their primary role is to detect and respond to potential threats, such as infections and allergens. When activated, mast cells release various substances, including histamine, which trigger an inflammatory response to neutralize the perceived threat.
Symptoms of Mast Cell Activation:

Recognizing the symptoms of mast cell activation is crucial for early detection and management. Common symptoms include:
– Flushing or hives
– Itching or rashes
– Swelling, particularly in the face or extremities
– Abdominal pain and cramping
– Diarrhea or constipation
– Headaches
– Fatigue
– Brain fog or difficulty concentrating
Understanding these symptoms is the first step toward seeking appropriate medical attention.
Diagnosis of Mast Cell Activation
Accurate diagnosis of mast cell activation is essential for effective management. The diagnostic process may involve:
- Medical History: The initial step involves a detailed discussion about your symptoms, their patterns, and potential triggers. This conversation helps in forming a hypothesis about mast cell involvement.
- Physical Examination: A thorough examination is conducted to spot visible signs of mast cell activation, such as skin changes or swelling, providing crucial physical evidence of the condition.
- Laboratory Tests: Blood and urine tests are crucial for detecting biomarkers indicative of mast cell activation, like elevated levels of tryptase or histamine, solidifying the diagnosis with concrete data.
- Skin Tests: To identify allergen sensitivities that may trigger symptoms, skin tests can be performed. While not all triggers are allergenic, this step can be informative for some individuals.
Triggers of Mast Cell Activation
Mast cell activation syndrome (MCAS) presents a unique challenge due to the broad spectrum of triggers that can provoke mast cell degranulation, leading to varied symptoms. Understanding these triggers is essential for individuals seeking to manage their condition effectively. This detailed overview encompasses dietary influences, environmental factors, emotional and physical stressors, and infectious agents, providing insight into the complex interplay of triggers in MCAS.
Dietary Influences
- Histamine-Rich Foods: Consuming foods high in histamine, including aged cheeses, fermented beverages, and certain meats, can intensify symptoms for those sensitive to histamine due to its role in triggering mast cell release.
- Food Additives: Artificial colors, preservatives, and flavor enhancers found in processed foods may initiate mast cell responses, underscoring the importance of a clean, whole-foods-based diet.
Environmental Factors
- Allergens: Pollen, mold spores, dust mites, and pet dander are common environmental allergens that can activate mast cells, leading to an inflammatory response.
- Insect Bites and Stings: The venom from insects such as bees, wasps, and mosquitoes can act as a potent trigger, causing localized or systemic mast cell activation.
- High Pollen Count: Seasonal variations leading to increased pollen levels can significantly impact those with MCAS, necessitating strategies for minimizing outdoor exposure during high pollen seasons.
- Sick Building Syndrome: Poor indoor air quality and exposure to mold in water-damaged buildings can trigger mast cell activation, highlighting the need for regular air quality assessments and mold remediation.
- Mold Toxicity: Specific toxins produced by mold, beyond general mold exposure, pose a severe risk for triggering mast cell activation, requiring thorough environmental cleaning and possibly relocation to a safer environment.
- Chemical Sensitivities: Sensitivity to chemicals in cleaning products, perfumes, personal care items, and even off-gassing from new furniture can provoke mast cell responses, advocating for the use of natural and unscented products.
Emotional and Physical Stressors
- Temperature Extremes: Sudden temperature changes, especially extreme heat or cold, can trigger mast cell activation, emphasizing the need for temperature regulation and acclimatization.
- Physical Stress: Physical trauma, including injury or overexertion during exercise, can lead to mast cell degranulation, suggesting a balanced approach to physical activity.
- Emotional and Mental Stress: Chronic stress, whether emotional, mental, or physical, can exacerbate MCAS symptoms. Implementing stress management techniques such as mindfulness, meditation, and cognitive-behavioral strategies can be beneficial.
Infectious Agents
- Lyme Disease and Bartonella: Infections, particularly those transmitted by ticks, such as Lyme disease and Bartonella, can trigger or worsen mast cell activation. Addressing these infections with targeted treatments is crucial for managing MCAS.
By recognizing and understanding the diverse triggers of mast cell activation, individuals with MCAS can take informed steps towards reducing flare-ups and improving their quality of life.
Gut Health and MCAS Management
After exploring the various triggers that can provoke mast cell degranulation, it’s important to consider the role of gut health in both histamine regulation and MCAS. The gut, armed with enzymes such as diamine oxidase (DAO), is essential for histamine breakdown. Conditions like leaky gut or dysbiosis can disrupt this balance, resulting in elevated histamine levels and exacerbated symptoms.
Furthermore, a healthy gut influences our immune responses and can affect the severity and development of allergies. Abnormal gut conditions may activate mast cells within the gut, leading to the release of inflammatory mediators and potentially intensifying MCAS symptoms.
Therefore, supporting gut health is vital in managing MCAS and histamine-related issues. This includes personalized dietary changes, gut-friendly supplements like probiotics, and other strategies to maintain a balanced gut environment. Addressing individual triggers and symptoms with the help of experts like Dr. Rasha El Naggar can lead to more effective management of these complex conditions.
Medications and Natural Treatments for MCAS
When it comes to managing Mast Cell Activation Syndrome (MCAS), an integrative approach that combines conventional medications with natural treatments can offer the most comprehensive relief. Understanding the role of each option empowers patients to make informed decisions about their health management strategies.

Medications for Mast Cell Activation Syndrome
1. Antihistamines
Function: These medications block the action of histamine, a chemical released during mast cell degranulation that contributes to many MCAS symptoms.
Types:
- H1 Blockers: Used to alleviate skin irritations, hives, and respiratory symptoms. Examples include cetirizine, loratadine, and diphenhydramine.
- H2 Blockers: Target gastric symptoms by reducing stomach acid and are helpful for symptoms like reflux. Famotidine and ranitidine are in this class.
Dosage Consideration: Standard doses may not be effective for all patients. A healthcare provider may recommend higher dosages to achieve symptom control.
2. Ketotifen
This is a second-generation antihistamine that also possesses mast cell stabilizing properties, making it a versatile choice for symptom management. It’s particularly useful for patients who don’t fully respond to standard antihistamine therapy.
3. Cromolyn Sodium
As a mast cell stabilizer, cromolyn sodium helps prevent the release of inflammatory and allergic mediators, thereby reducing symptoms like diarrhea, abdominal pain, and skin rashes. It is available in oral forms for systemic treatment and inhaled forms for respiratory symptoms.
4. Benzodiazepines
Primarily used for their anxiolytic and central nervous system depressant effects, benzodiazepines can also help stabilize mast cells by acting on GABA receptors.
Consideration: They are typically used with caution due to their potential for dependency and withdrawal issues.
5. Montelukast (Singulair)
As a leukotriene receptor antagonist, montelukast helps control inflammatory responses in the lungs and nasal passages, reducing asthma-like symptoms and allergic rhinitis.
6. Inhalers
Bronchodilators: Albuterol and similar medications can relieve bronchospasm associated with MCAS.
Corticosteroid Inhalers: These reduce inflammation in the airways and are used for chronic management of respiratory symptoms.
7. Epinephrine Auto-Injectors (EpiPens)
Emergency Use: For immediate treatment of anaphylaxis, a severe allergic reaction that can occur with MCAS. Patients are advised to carry an EpiPen at all times.
8. Low-Dose Naltrexone
Typically used for pain disorders and opioid overdoses, low-dose naltrexone has been found to have anti-inflammatory effects and may be beneficial for some MCAS patients.
9. Corticosteroids
In cases of severe symptoms or acute flares, short-term use of corticosteroids may be recommended to rapidly suppress the immune response.
Caution: Due to potential side effects with prolonged use, corticosteroids are typically reserved for short durations.
Natural Interventions for Mast Cell Activation Syndrome
While medications form the cornerstone of symptom management in Mast Cell Activation Syndrome (MCAS), natural interventions can play a significant role in an integrative management plan. These natural strategies aim to complement pharmacological treatments, offering additional relief and support to individuals with MCAS. Here’s an overview of the natural interventions that may help stabilize mast cells and manage symptoms:
- Nutraceuticals
- Vitamin C: This essential nutrient acts as a natural antihistamine. It can help degrade histamine and support the immune system.
- Quercetin: A flavonoid with antioxidant properties, quercetin is known to help stabilize mast cells and reduce the release of histamine and other inflammatory substances.
- Omega-3 Fatty Acids: Found in fish oil and flaxseed oil, omega-3s are renowned for their anti-inflammatory effects and may help modulate the immune response in MCAS.
- Bromelain: An enzyme from pineapple that has anti-inflammatory properties and may assist in breaking down histamine.
- Curcumin: The active compound in turmeric, curcumin, has potent anti-inflammatory properties that may be beneficial for reducing mast cell-mediated inflammation.
- Herbal Supplements
- Nettle Extract: Stinging nettle is sometimes used as a natural antihistamine and anti-inflammatory agent.
- Butterbur: Known for its use in reducing the frequency and severity of migraines, butterbur may help manage similar symptoms in MCAS.
- Ginger and Peppermint: These herbs are commonly used to soothe digestive issues, a frequent concern for individuals with MCAS.
- Dietary Adjustments
- Low-Histamine Diet: Eliminating or reducing foods high in histamine can help decrease the overall histamine burden and potentially lessen MCAS symptoms.
- Elimination Diet: Gradually removing and reintroducing foods can help identify specific dietary triggers for symptoms. Working with a healthcare professional or a registered dietitian can help create a personalized diet plan
- Lifestyle Modifications
- Stress Management: Techniques such as meditation, yoga, and deep breathing exercises can help reduce stress, which may trigger mast cell activation.
- Environmental Controls: Using HEPA filters to purify air and choosing hypoallergenic bedding and clothing can minimize exposure to environmental triggers.
- Appropriate Clothing: Wearing loose-fitting, breathable clothing can help prevent overheating and reduce the risk of triggering symptoms.
- Regular Exercise: Engaging in regular, moderate exercise can have positive effects on overall health and may help manage stress. However, it’s important to consult with a healthcare provider before starting any new exercise regimen
- Gastrointestinal Support
- Probiotics and Prebiotics: Aiming to balance gut flora, these supplements can support digestive health, which is often affected in MCAS.
- Fiber: Adequate fiber intake helps maintain bowel regularity, potentially easing gastrointestinal symptoms associated with MCAS.
- Hydration and Electrolytes
- Adequate Fluid Intake: Staying well-hydrated is crucial for overall health and can support the body’s detoxification processes.
- Electrolyte Balance: Ensuring a proper balance of electrolytes through diet or supplements can help manage symptoms like dehydration and fatigue.
When exploring natural interventions for MCAS, individual responses can vary. That’s why a personalized approach, crafted with a healthcare provider skilled in both conventional and natural remedies, is critical. Dr. Rasha El Naggar specializes in such personalized healthcare, ensuring the safe and effective integration of natural treatments for MCAS.
With Dr. Rasha’s expertise, patients can confidently incorporate natural strategies into their overall treatment plan, potentially improving their quality of life and managing MCAS symptoms more effectively
To Conclude
As we conclude our exploration of Mast Cell Activation, it’s crucial to recognize the profound impact this condition can have on the lives of those affected. While mast cells are the vigilant defenders of our immune system, their occasional overzealous responses can lead to a spectrum of symptoms, creating challenges for individuals striving to maintain a sense of normalcy.
Understanding the intricacies of mast cell activation is akin to deciphering the language of your body’s defense system. The symptoms, ranging from skin reactions to digestive issues, are like messages that something is amiss. Diagnosing mast cell activation is crucial, relying on detailed medical histories, physical exams, and specific tests to guide personalized treatment. Beyond diagnosis, proactive management through lifestyle changes, dietary adjustments, and stress reduction plays a key role in mitigating symptoms.
Medications like antihistamines, mast cell stabilizers, and corticosteroids are vital, reflecting medical advancements in offering relief. Education is essential, enabling patients to understand their condition and become active participants in their care. Regular communication with healthcare providers ensures treatment plans remain effective and responsive to patients’ needs.
By understanding the symptoms, triggers, and available treatments, patients can take proactive steps to improve their quality of life. If you suspect mast cell activation, don’t hesitate to consult with Dr. Rasha El Naggar for personalized guidance and support.
Visit Etara Wellness for a comprehensive evaluation. Contact Dr. Rasha El Naggar for a professional and thorough assessment. Book your appointment now for dedicated care and expert guidance.
CLAIM YOUR 15 MINUTES FREE PHONE CALL
Disclaimer: This content is for educational purposes only and not intended as medical advice. Consult a healthcare professional for any medical concerns.